Written by Sophia Zaragoza, L.A.T., ATC
Athletic trainers (ATs) have the privilege of working with athletes during the season, pre-season, and post season. ATs must review best practices and prepare for emergent scenarios. Beyond their orthopedic wheelhouse, there is an appreciation for general medical disorders. Among endocrine disorders, diabetes is prevalent in the athletic population at all levels of participation. It is imperative to proactively educate on recognition and management to deliver outstanding healthcare.
The Difference Between Type II and Type I Diabetes Mellitus
Diabetes Mellitus (DM), a common metabolic disorder, affects approximately 38 million Americans (1 in every 10 people). Of these reported cases, approximately 90-95% are Type II, while the remaining 5-10% are Type I.
Type II diabetes, characterized by insulin resistance, leads to a buildup of glucose in the bloodstream and often develops due to poor diet and lack of exercise.
While insulin, a hormone that regulates blood glucose, may be produced in sufficient quantities, the body’s cells are not responsive to its signal to move sugar into the cells. Type II DM can often be managed through diet and lifestyle changes.
Type I diabetes, on the other hand, is not preventable and can occur at any age. It is an autoimmune disorder in which the body either attacks its insulin-producing cells or does not produce enough insulin. This condition must be managed with external insulin therapy.
Although both types of diabetes affect energy (sugar) metabolism, there are significant differences in their management.
Managing Diabetes with Athletes: Importance of Tailoring Care Plans for Diverse Sports and Activities
Understanding that diabetes is a metabolic disorder related to glucose, an athlete’s or physically active individual’s care plan must take into account the energy demands of their sport or activity. For example, the energy needs of a baseball first baseman are different from those of a rugby winger or a swimmer competing in a 400m event.
While athletes with diabetes are already at a higher risk for hypo- and hyperglycemic events, this risk is further increased if there is not a well-managed or clearly communicated plan of care. Mismanagement can lead to catastrophic events, making it imperative to recognize symptoms, manage them appropriately, and communicate thoroughly. Explore the common signs, symptoms and management tips to be aware of as an athletic trainer caring for Type I, and Type II athletic populations down below.
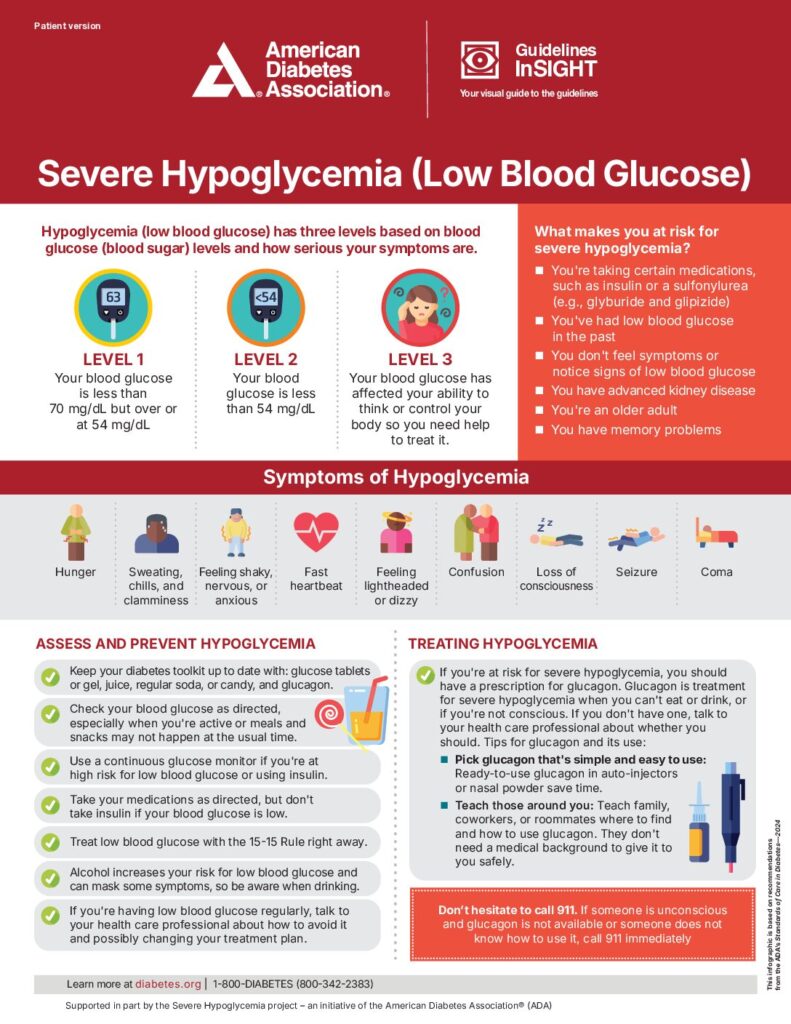
Hypoglycemia: Low Blood Sugar (<70 mg/dL)
Signs and Symptoms
- Tachycardia
- Sweating
- Palpitations
- Hunger
- Nervousness
- Headache
- Trembling
- Dizziness
Management
15/15 Rule:
- Administer 15 grams of carbohydrates to increase blood glucose.
- Check blood glucose after 15 minutes. If it is still <70 mg/dL, administer another 15 grams.
- Repeat steps 1 and 2 until blood glucose reaches at least 70 mg/dL, then eat a small meal or snack to prevent another hypoglycemic event.
Note: Avoid consuming more than 15 grams of carbohydrates per 15 minutes to prevent excessive blood glucose spikes. Document the hypoglycemic event and carbohydrate intake. If blood glucose remains low, continue treatment and activate EMS.
*The 15/15 Rule is a primary method for treating hypoglycemia when the patient is conscious and able to swallow. If the athlete experiences an altered state of consciousness or cannot swallow, emergency action is required.
Moderate-Severe Hypoglycemia
Signs and Symptoms
Moderate: Below 54 mg/dL
- Dizziness
- Sleepiness
- Weakness
- Irritability
- Difficulty speaking
- Confusion
Severe: Below 40 mg/dL
- Disorientation/Altered consciousness
- Seizures or convulsions
- Sleepiness
- Coma
Management
- Activate EMS immediately.
- Do NOT inject insulin.
- Do NOT provide food or fluids (choking hazard if altered LOC).
Glucagon Administration:
- Injectable: Administer into the buttock, arm, or thigh, following kit instructions.
- Inhalable: Follow package instructions to administer through the nostril.
- Once the individual is stable, they should consume carbohydrates as soon as they are able.
Interested In Learning More About How To Manage Hypo- and Hyperglycemia in Your Athletes?
Diabetic events can happen unexpectedly, but with proper preparation and management, you can ensure your athletes stay safe and perform at their best. If you're interested in exploring additional resources and insights on how you can support diabetic athletes, JAG PT's athletic training services are here to guide you and your team.
Protect Your Athletes: Schedule An Appointment with JAG Physical Therapy:
If you notice an athlete struggling with an injury or experiencing discomfort, it's crucial to take action immediately. At JAG Physical Therapy, our expert athletic trainers provide tailored care and support to help athletes recover safely. Schedule a training session with one of our experts or contact JAG Physical Therapy today!